Build with Axial: https://axial22.axialvc.com/
Axial partners with great founders and inventors. We invest in early-stage life sciences companies such as Appia Bio, Seranova Bio, Delix Therapeutics, Simcha Therapeutics, among others often when they are no more than an idea. We are fanatical about helping the rare inventor who is compelled to build their own enduring business. If you or someone you know has a great idea or company in life sciences, Axial would be excited to get to know you and possibly invest in your vision and company . We are excited to be in business with you - email us at info@axialvc.com
There is a large opportunity to transform immune cells in situ to treat cancer and more. One limitation of CAR-T cell therapy is the phenotypic diversity of tumors, which means some cancer cells are not recognized by the targeting receptors and as a result, form immune escape variants. Programming lymphocytes with chimeric antigen receptors (CAR) that recognize different tumor antigens could address this problem, but generating a spectrum of fully comprehensive T-cell variants is not practical using current ex vivo methods. On the other hand, for example, injectable reagents to program T-cells in vivo could offer a simple way to rapidly generate immunity against any targetable tumor antigen. The Mooney Lab at Harvard/Wyss Institute has the best IP here. Multiple T-cell specificities can be fine-tuned to match the antigenic fingerprint of each patient’s tumor. Another set of advantages for in vivo cell therapies are removing supply chain issues and the preconditioning step (which is also an advantage for B-cell therapeutics).
Key components for an in vivo cell therapy are:
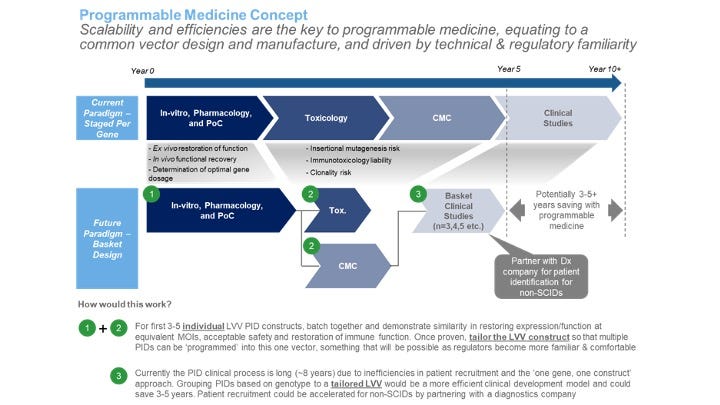
Delivery vector - lentiviral (Umoja’s approach), nanoparticles, HSVs. They need to have safety, capacity to be easily manufactured, and ideally just require a countable number of doses.
Payload - the actual cargo transformed into an immune cell and has to be able to be packaged into the vector
Shared biology across payloads - so for a given vector, the likelihood of success across payloads increases over time
The 2 current leaders in the field are Interius Biotherapeutics from Saar Gill’s Lab at Penn and Umoja Biopharma mainly from Michael Jensen’s work at Fred Hutch. Yvonne Chen’s Lab at UCLA also has IP to start a NewCo in this field as well. She’s a superstar.
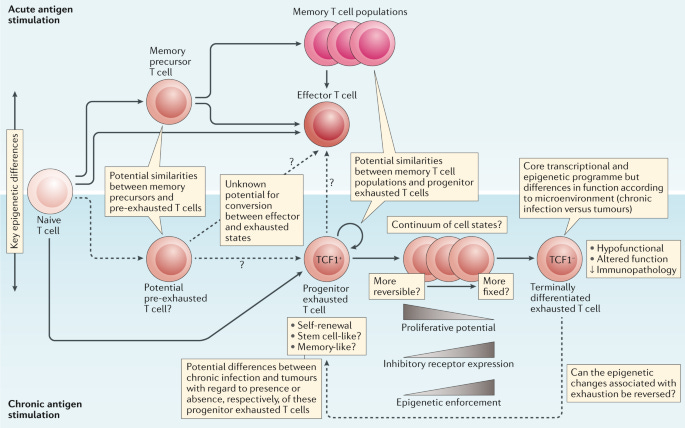
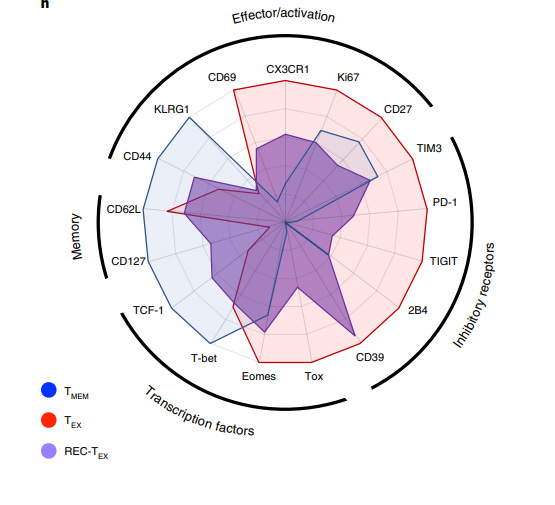
An important thesis in cell therapies is finding the active ingredient, both activating and inhibitory. Exhausted T-cells (Tex) come in 2 main subsets: progenitor and terminally differentiated. Tex’s are often functional but are in a stalemate with either a pathogen or cancer. This stalemate provides an opportunity to reverse exhaustion. There is a massive need for a more complete understanding of the number of truly distinct subsets of exhausted T cells, their diversity and underlying epigenetics. T-cell exhaustion, usually manifests with several characteristic features, such as progressive and hierarchical loss of effector functions, sustained upregulation, and co-expression of multiple inhibitory receptors, altered expression and use of key transcription factors, metabolic derangements, and a failure to transition to quiescence. These parts represent large opportunities to explore to design new cell therapies.
For example, Lyell is using c-Jun overexpression from the Mackall Lab at Stanford to reverse or at least resist exhaustion. Their cell therapy relying on this technology recently cleared IND for treating solid tumors - https://ir.lyell.com/news-releases/news-release-details/lyell-immunopharma-announces-fda-clearance-its-ind-lyl797-car-t Progress here will be exciting to track.
Other work in the field is:
IP out of Poojary Lab deleting Cbl-b to reverse T-cell exhaustion
Wherry Lab at Penn discovered the transcription factor, TOX as a mediator of T-cell exhaustion - https://pubmed.ncbi.nlm.nih.gov/31207603/
Oldstone Lab at Scripps for small molecule screening of reversing T-cell exhaustion - https://www.cell.com/cell-reports/pdf/S2211-1247(19)31452-4.pdf
A compelling case study for building new technologies to probe exhaustion that can set up successful in vivo cell therapies comes out of the Wherry Lab: Epigenetic scarring of exhausted T cells hinders memory differentiation upon eliminating chronic antigenic stimulation - https://www.nature.com/articles/s41590-021-00975-5
The paper studied whether exhausted CD8+ T-cells (Tex) can recover normal functions if they are no longer exposed to a virus. This approach can be extended to tumor exposure.
In vivo, the group used the mouse virus, LCMV to initiate T-cell exhaustion. After transplantation of Texs into non-infected mice without antigen exposure, most Texs died (>99%) but the few that survived recovered some gene expression profiles similar to normal memory T-cells but overall remained exhausted with highly stable epigenetic changes.
Work like this acts as a starting point to understand what causes T-cell exhaustion and uncover new ways to reverse it. For an in vivo therapy, this data is essential to design medicines that can deal with tumor evasion and take full advantage of transforming immune cells in situ with the goals of expanding the indications that can be treated with potentially curative cell therapies and increasing patient response rates.
We are making a request for talent here. Whether you’re an inventor, an operator, product manager, engineer, and more, cell therapies need fresh approaches with a focus on new platforms and scalable business models. Axial will provide investment as well as our network of founders and executives and internal team of venture partners. In particular, we are excited about epigenetic reprogramming to convert Texs into effector/memory T-cells in vivo. If you’re interested, please email us at info@axialvc.com